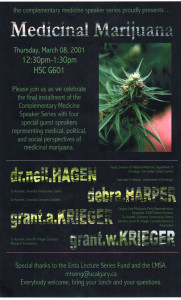
Complementary Medicine Speaker Series
Medical Marijuana
University Of Calgary
March 8, 2001
I would like to thank Michael Tseng very much for having the foresight to create this remarkable opportunity for all of us. My name is Debra Harper and it is a pleasure to be here today to participate in this discussion.
Last summer, I organized an Information Night for the Universal Compassion Centre, a non-profit society which provided cannabis to members with medical conditions; because I saw a similar need for those of us involved with medical marijuana to begin to publicly inform the community, medical establishment, and government officials about this herb. Due to many difficulties, the UCC is now dormant, but I’m involved in new ventures to help facilitate cannabis therapy, and believe forums such as this, initiated by other stakeholders, is definitely a sign of the times.
Indeed, we are in a new century, a new age, and the face of traditional Western medicine is slowly changing. The aging boomer population are looking for choices that suit their desire for safer, natural remedies to treat their ailments. Open-mindedness about complementary medicines will benefit the medical profession and patients alike, and it is very encouraging to see you here today to as we discuss this particularly controversial medicine known as cannabis or marijuana.
This herb has been used for thousands of years to treat many different afflictions and the amount of information available is so encompassing, I could not possibly touch on all aspects of this plant, so I will limit my presentation to dealing with current issues and how they will affect everyone – and relying on handouts to provide additional information and services available.
This summer – under pressure from the courts – the government will be announcing new measures on how the sick can access cannabis. Right now, it has been estimated over 300 people across Canada have been approved for a Section 56 exemption which gives them the legal right to use it, with over a thousand more applications in the system; mostly for pain management.
Physicians must complete extensive paperwork to meet Health Canada requirements on behalf of their patients, who once approved, are required to grow their own supply. The courts recognized that this does not address many legal and health issues and although it is unknown at this time how streamlined the process will become, one thing is certain; doctors will continue to be required to oversee their patients cannabis use.
Many doctors and patients are uncomfortable with cannabis being regulated through the medical profession, partly because, right now, it is frowned upon by the College of Physicians and Surgeons, and even Health Canada itself, for doctors to condone or write prescriptions, and that mind-set will not change overnight – and partly because it seems somewhat misplaced when you think that people do not go to their physicians for acupuncture, massage, herbal or other complementary therapies or medicines. But what we will learn about the intricacies of cannabis therapy through doctor-patient dialogue will enable us to put forward recommendations for future improvements, such as regulating it more appropriately under the newly established Office of Natural Health Products.
Just to give you an idea of what is in store, Canada’s Centre for Addiction and Mental Health published a survey in the Canadian Medical Association Journal that found 1.9% of the respondants, which translates to over a half-million Canadians, reported using marijuana for medical reasons, mostly pain and nausea. With recent polls indicating 92% of Canadians support marijuana for medical purposes (1), and once it is recognized and accepted by politicians and physicians as a legitimate form of medicine for many ailments, the number of people discussing cannabis with their doctors will rise considerably.
In the meantime, most people still access cannabis through the blackmarket, which, for many reasons is extremely problematic. The financial strain placed by exorbitant prices, combined with breaking the law and the inherent consequences; causes undue stress and hardship on already sick people and their families.
Also, It is believed that different strains have different effects or degrees of successfully easing symptoms, yet strain identification is usually not possible through the local dealer, so many patients do not have access to strains which could be more effective for their ailment.
The quality of street cannabis is also questionable in terms of impurities caused by inexperienced and /or greedy growers, and this can have dire consequences in someone with a suppressed immune system, while being generally unhealthy for others.
This is a world-wide problem as Australian Dr. Lisa Jackson pointed out in her submission last month to her government, entitled, ” A Response to the Report of the Working Party on the Use of Cannabis for Medical Purposes”.(2) She stated, “For no other medicine are patients or their caregivers expected to, produce it themselves, or purchase it from the black market, and to manage quality control. The production and supply of medical cannabis needs to be addressed legislatively, and with practical common sense”. She adds, “Knowing that some patients may be particularly susceptible to the micro-organisms sometimes present in cannabis, and to provide no realistic supply, no access to quality control, and leaving them exposed to the risks of the black-market, could be seen as negligent.”
Our government announced it will be providing a safe, clean product to those involved in the upcoming clinical trials and exemptees, but this does not help the vast majority of users, and once new regulations are in place, it is highly doubtful proper provisions will address this situation.
From a doctor’s perspective, aside from lobbying for change, not much can be done about the supply situation for their patients who are not in an approved government program, but continue to use it anyway. Perhaps becoming knowledgeable and approachable, and offering advise on different methods of ingestion, possible benefits and risks, strain selection, and by supporting their right to access cannabis through compassion clubs by completing the necessary forms, which generally only requires a signature verifying the patient has the medical condition they list. This would aid the patient greatly – both physically and psychologically.
I sympathize with doctors – they are forced into a tough spot between politics and the health of their patients. As Dr. Keith Martin stated during the debate to legalize cannabis for medicinal purposes in the House of Commons on May 25/99, “We do not know if the effects of marijuana consumed under those conditions are due to a medical or therapeutic effect due to the intrinsic pharmaceutical property of marijuana or whether this is a placebo effect. As a physician, I personally do not care. In my view, if somebody is dying they should be able to participate in whatever it takes to relieve their suffering as long as it does not hurt anybody else. “(3)
To quote Dr. Jackson again, “The fact that so many patients still choose to use cannabis for its therapeutic effects, despite its illegality, is testimony to both this plants qualities as a medicine and patients right to choose. Obviously patients should not be persecuted for using a natural medicine to improve their quality of life.”
I truly hope physicians choose compassion and common sense in their patients care because, the patient’s right to choice in medicine must prevail over political and corporate interests.
Debra Harper
Cited:
(1)“Two-thirds favour decriminalizing pot” – The National Post, May 15, 2000
(2)Response to the NSW Working Party on the Use of Cannabis for Medical Purposes – Dr. Lisa Jackson
(3) House of Commons Debate
Epilogue
All the concerns raised in this lecture proved to be true and doctors are still the reluctant gatekeepers today. The new regulations introduced at the time did not adequately address the problems.